HPRC continues its series on Pain Management with an article on epidural steroid injections (ESIs), which involve injections of pain medication around the spinal nerve roots. They are done by qualified healthcare providers for short-term relief of back and neck pain. They also can help doctors diagnose some types of pain.
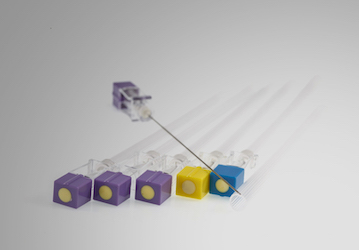
Epidural steroid injections (ESIs)—a treatment for short-term relief of back and neck pain—involve injecting a small amount medication into the space surrounding the spinal canal. This space, called the “epidural space,” contains the spinal cord and spinal nerve roots. The “dura” is a tough membrane that covers and protects the spinal cord, so “epi-dural” really means “outside the dura.” Sometimes medication can be placed next to nerve roots as they exit the spinal cord around the vertebrae (the bones of the spine).
ESIs must be performed by qualified healthcare providers. They may consist of either steroid or anesthetic medications. Steroid medications reduce inflammation and, hopefully, pain. Anesthetic medications block pain signals to the brain but do not reduce inflammation. When the pain radiates to the legs or arms, ESIs sometimes help doctors pinpoint the causes of the pain. In addition, imaging techniques such as fluoroscopic guidance (continuous X-ray) and ultrasound are sometimes used to provide more accurate needle placement of the steroid to reduce side effects.
What We Know
ESIs are helpful for certain types of spinal conditions. For example, ESIs appear to be better for neck pain from herniated disks (when the disks between the spinal bones rupture) than for spinal stenosis (narrowing of the space around the spinal cord). Also, anesthetic combined with anti-inflammatory medication seems to work better for neck pain than either medication alone.1 There is some support for the use of ESIs with mid-back pain2, but there is not enough evidence at this time, and more research is needed.
Many people find ESIs helpful for low-back pain. They can reduce the pain related to low-back herniated disks and spinal stenosis in some people.3,4 As mentioned above, ESIs appear to be more helpful when the pain is from herniated disks rather than spinal stenosis.5 There is some evidence that people who have ESIs for pain from spinal stenosis have worse outcomes than those with spinal stenosis who do not have ESIs.6
ESIs offer some pain reduction but do not work as well as other treatments such as diskectomy for herniated disks.7 It is not clear how well ESIs work for general low-back pain. Many doctors do not recommend ESIs for non-specific back pain, given that there are risks associated with the procedure (see more below).8
Overall, it appears that ESIs can sometimes offer short-term relief for certain back/neck pains, but their long-term effects and cost-effectiveness are debated.9 ESIs often are combined with different types of treatments for chronic pain. The National Institutes of Health reports that ESIs are generally safe when performed by doctors who are trained pain specialists. They are the most common procedure performed in pain clinics throughout the United States.
Concerns
ESIs usually are used after less-invasive pain treatments such as oral medications and physical therapy have not worked. Common side effects are soreness, redness, and bruising around the injection site. Minor side effects also include dizziness, headache, nausea, and allergic reactions to the medicine. Severe side effects are rare but include infection, bleeding around the spinal cord, and when done in the neck, spinal cord damage. ESIs should only be given a few times a year because too much steroid can cause bone, fat, and muscle loss. They also can disrupt hormone balances. A review of the research demonstrated that ESIs should be "administered cautiously, with careful monitoring for systemic side effects."10
Debrief (Military Relevance)
Back, neck, and arm/leg pain from herniated discs are common in service members because of the significant physical demands of military service. ESIs are being used in the military to treat back and neck pain as part of a comprehensive pain management plan (for more information on how the VA and DoD treat pain, check out HPRC's FAQ). In combination with other pain treatments, they appear to be helpful at getting service members back to duty.11 Overall, ESIs provide at least short-term relief that allows service members to engage in longer-term pain management techniques such as stretching, exercising, and physical therapy.
Note: This InfoReveal is an educational overview that describes the use of epidural steroid injections (ESIs) as a strategy for pain management; it is not a comprehensive review of the current state of the research.
This InfoReveal was created in collaboration with the Defense & Veterans Center for Integrative Pain Management.